How Can You Identify A Few Tell-tale Signs Of Depression In People Around You?
Depression (major depressive disorder or clinical depression) is defined as a common but serious mood disorder. It causes severe symptoms that affect how you feel, think, and handle daily activities, such as sleeping, eating, or working. To be diagnosed with depression, the symptoms must be present for at least two weeks.
You can identify if someone around you is suffering from Depression in the following ways:
Major Depressive Disorder: Diagnostic Criteria
1. Five (or more) of the following symptoms have been present during the same 2-week period and represent a change from previous functioning: at least one of the symptoms is either (1) depressed mood or (2) loss of interest or pleasure.
Note: Do not include symptoms that are clearly attributable to another medical condition.
2. Depressed mood most of the day, nearly every day, as indicated by either subjective report (e.g., feels sad, empty, hopeless) or observation made by others (e.g.appears tearful). (Note: In children and adolescents, can be irritable mood.)
3. Markedly diminished interest or pleasure in all, or almost all, activities most of the day, nearly every day (as indicated by either subjective account or observation).
4. Significant weight loss when not dieting or weight gain (e.g., a change of more than 5% of body weight in a month), or decrease or increase in appetite nearly every day.
(Note: In children, consider failure to make expected weight gain.)
5. Insomnia or hypersomnia nearly every day.
6. Psychomotor agitation or retardation nearly every day (observable by others, not merely subjective feelings of restlessness or being slowed down).
7. Fatigue or loss of energy nearly every day.
8. Feelings of worthlessness or excessive or inappropriate guilt (which may be delusional) nearly every day (not merely self-reproach or guilt about being sick).
9. Diminished ability to think or concentrate, or indecisiveness, nearly every day (either by subjective account or as observed by others).
10. Recurrent thoughts of death (not just fear of dying), recurrent suicidal ideation without a specific plan, or a suicide attempt or a specific plan for committing suicide.
The symptoms cause clinically significant distress or impairment in social, occupational, or other important areas of functioning.
The episode is not attributable to the physiological effects of a substance or to another medical condition.
Note: Criteria A-C represents a major depressive episode.
Note: Responses to a significant loss (e.g., bereavement, financial ruin, losses from a natural disaster, a serious medical illness or disability) may include the feelings of intense sadness, rumination about the loss, insomnia, poor appetite, and weight loss noted in Criterion A, which may resemble a depressive episode. Although such symptoms may be understandable considered appropriate to the loss, the presence of a major depressive episode in addition to the normal response to a significant loss should also be carefully considered. This decision inevitably requires the exercise of clinical judgment based on the individual’s history and the cultural norms for the expression of distress in the context of loss.
- The occurrence of the major depressive episode is not better explained by schizoaffective disorder, schizophrenia, schizophreniform disorder, delusional disorder, or other specified and unspecified schizophrenia spectrum and other psychotic disorders.
- There has never been a manic episode or a hypomanic episode.
Note: This exclusion does not apply if all of the manic-like or hypomanic-like episodes are substance-induced or are attributable to the physiological effects of another medical condition.
Case Study:
“Through my work experience in Counseling, I have had this one case where “my clients who were a young couple were treated for Depression – Shalini & Rahul (names changed.) Shalini was angry with Rahul because he had been (in her opinion) distant and unloving towards her in recent weeks. No matter how hard she tried to please him, nothing seemed to work. She began wondering whether he had lost interest in her. After I asked Rahul certain key questions, it became clear that he had gradually become depressed. Hence, had lost interest in pretty much everything that had previously given him pleasure including Shalini. Once Rahul’s depression was adequately treated, he became the warm, loving and attentive man with whom Shalini had fallen in love & married. But, how does someone know when a loved one is slipping into depression?
In this case, Shalini had seen a drastic change in Rahul’s thought process, behaviour and mood. He lost interest in things which he liked doing before and was in constant state of being low regardless of what Shalini would do uplift his moods”.
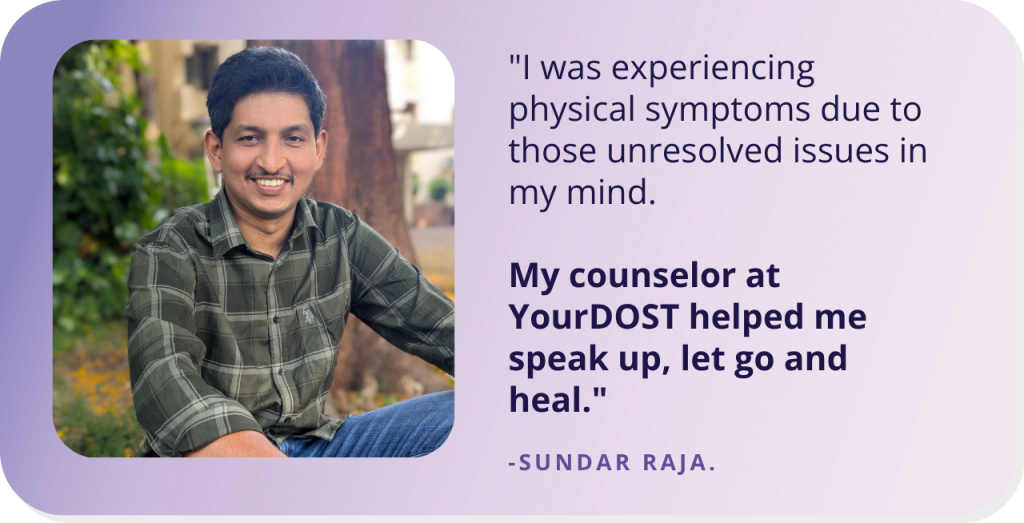
Are you someone who has gone through a difficult phase and emerged stronger and better, with some professional help? Share your story with us to encourage thousands of others who might be struggling. click here to submit your story.